Illustration by Armine Shahbazyan.
Thirty years after independence, Armenia’s healthcare system has achieved some successes and reached various milestones, but overall remains inefficient, mismanaged, and incapable of serving some of the basic healthcare needs and obligations of Armenian society. With a maldistribution of infrastructure and human resources, weak government oversight, socio-economic imbalance, and low public financing, Armenia’s healthcare system struggles to fulfill its Constitutional obligations. This is compounded by underlying failures to meet certain ethical duties, along with obligations to international initiatives.[1]
Intertwined within such broader problems is the inefficient expenditure and waste in the healthcare system. While a great deal of money is spent on healthcare in Armenia, a hefty portion of this is from out-of-pocket rather than public spending. The result has been corporate profits and indiscriminate spending at the expense of public health and citizen well-being, a concept known as “health pollution.” The extant literature on healthcare and public health demonstrates that the solutions to the sorts of complications that Armenia’s health system suffers from can only be remedied by building a robust and sustainable system. Ad-hoc methods, or temporary solutions, not only fail to improve the healthcare system, but may also produce a reverse effect, thus reinforcing the inherent structural limitations that the system suffers from. In more simple terms, a damaged system cannot be cured by using bandaids: a comprehensive and transformative approach is required.
Collectively, Armenia’s healthcare system, for the last three decades, has suffered from lack of vision, inchoate strategic planning, poor quality, and widespread corruption and nepotism. The country’s healthcare system, broadly speaking, is inefficient, relatively ineffective, and for these reasons, has produced a less healthier population. It suffers from fragmentation, redundancy, structural miscommunication, and flawed infrastructural design. To this end, the need for widespread healthcare reforms must prioritize a strong relationship between citizen health, demographics, and a qualitatively improved healthcare system. More specifically, unless Armenia’s quality of healthcare improves, all other endeavors, from enhancing the quality of medical equipment to increasing the number of healthcare professionals, will not alleviate the systemic shortcomings that Armenia’s public health faces.
In an expansive article published with the International Journal for Equity in Health, complications and shortcomings in Armenia’s healthcare system, specifically the factors contributing to its inequalities, were defined by the following metrics: 60% due to financial barriers, 40% due to lack of trust in healthcare professionals, 28% due to insufficient quality of diagnostic examinations, and 10% due to absence of modern equipment.[2] As the empirical findings demonstrate, qualitative improvements in Armenia’s healthcare system remain specific to the shortcomings within the system itself. Quantitative improvements in numbers of medical equipment, healthcare professionals, or access to healthcare—as research demonstrates—will not address the structural and systemic problems that Armenia’s healthcare sector suffers from. Unless quality is improved, all other factors will suffer from inefficiency and lack of efficacy. As the Commission on High-Quality Health Systems noted in a renowned study by Lancelot Global Health: “Providing health services without guaranteeing a minimum level of quality is ineffective, wasteful and unethical.”[3]
Healthcare is an expensive commodity, and it is to be expected that a low-income country like Armenia is not capable of fully covering all health expenditures for its population. As successful healthcare reforms in different societies have demonstrated, the solutions lie in methodical and fair rationing, followed by developing an efficient, high quality, and cost-effective healthcare system. As healthcare reforms and quality of healthcare increases, Armenia can then continue to minimize rationing, as the qualitatively improved health care system, due to efficient and cost-effective mechanisms, begins addressing the health demands of society. In this context, considering Armenia’s economic limitations, healthcare reforms must primarily concentrate on optimization: developing an efficient and lean healthcare system with robust government oversight and emphasis on quality.
Quality of Care as Sustainable Solution
As scholarship on the subject has demonstrated, quality of healthcare supersedes other factors in the broader policy implications of developing a sustainable system. While, indeed, quantitative metrics such as number and types of healthcare professionals and equipment are important, these remain secondary to a systemic improvement of quality in Armenia’s case. Namely, chronic and latent problems cannot be solved without systemic solutions. As an example, one may consider the 2018 study in the journal Lancet which demonstrated that of all the preventable deaths in Armenia, more of them were due to patients receiving care, but that care being of poor quality, rather than because of non-utilization or a lack of access to healthcare.
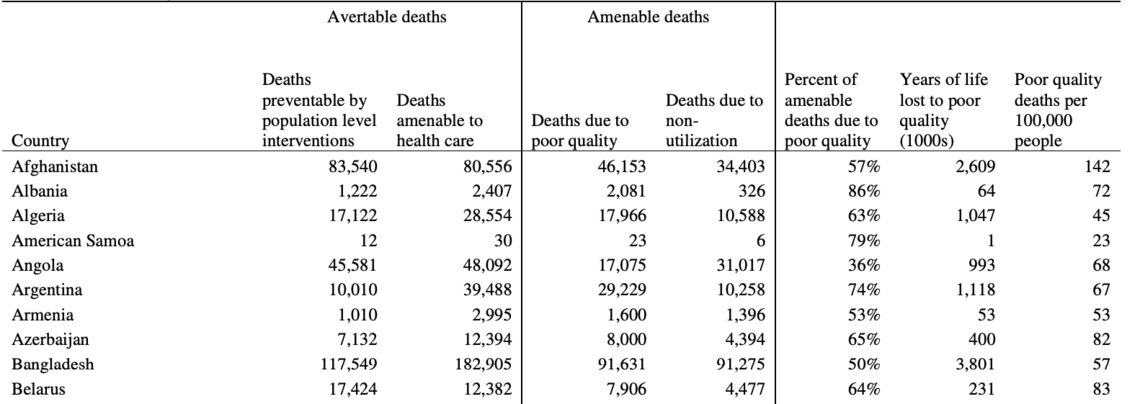
Source: The Lancet, Volume 392, Issue 10160, Pp. 2023-2012, November 17, 2018
In this context, “more” has resulted in “less,” for the lack of quality in the former is producing outcomes that are detrimental to the latter.
As such, more healthcare does not mean better healthcare, and to this end, more low-quality care actually results in higher proportions of detrimental outcomes. Furthermore, findings demonstrate that healthcare workers in well-equipped facilities often provide poorer care and vice versa. While this may come off as counter-intuitive to many, the empirical referents remain unchallenged: throwing material resources at a problem is not going to solve the problem if the problem itself is not hinged on material resources. Thus, more doctors, more medical equipment, and even more Diaspora money, for example, is not going to solve the problems in Armenia’s healthcare system, and perhaps to the contrary, it may actually, although unintentionally, contribute to the problematic path-dependency that the health system suffers from.
This stipulates that change is required in the way healthcare is conceptualized and comprehended both in Armenia and the Diaspora. In this context, it is fundamental to accept the fact that the solutions to most of Armenia’s healthcare problems lie not in providing more care, but rather making drastic improvements in quality of care. In fact, over-emphasis on “more,” such as more hospitals, more doctors, or more “high tech” equipment, can, and in Armenia’s case does, have a negative impact on its ability to deliver better quality care to its population. Studies have repeatedly shown that facilities, or the level of equipment within these facilities, have very little to do with the provision of high-quality care. To this end, Armenia’s healthcare culture, and the public understanding of health, must undergo a certain paradigm shift. And this roadmap was provided a long time ago by the father of healthcare quality Avedis Donabedian, who decades ago realized that quality is dependent on the triad of structure, processes and outcomes. Thus, it is essential that we concede that structure, alone, will get us nowhere. Yet the reality, however, has been precisely that: structure has been and remains the focus of the Armenian nation’s approach to the Republic’s health system. For this reason, very little has been done to introduce quality assurance, improvement, monitoring and evaluation mechanisms on a systemic level; to the contrary, we have continued to build and maintain hospitals at a mind boggling rate.
Infrastructure and Human Resources
A similar symptom of this broader problem can also be observed when it comes to infrastructure and human resources. Consider, for example, how numerical superiority in the number of hospitals does not translate to better public health or improvements in healthcare. Yerevan, proportionally speaking, has 41 hospitals per million people, while Los Angeles has 12 hospitals per million people. Geographically, Yerevan has 47 hospitals per 100 mile radius, while Los Angeles has 2 hospitals for the same radius. The qualitative level of care between the two cities is clearly not comparable, yet purely observed through the lens of “more” infrastructure, Yerevan has “more” accessible health facilities for its citizens, per capita, than Los Angeles. But as research shows, having “more” does not translate into “better;” rather, it produces an inverse-effect: in the case of Armenia, “more” translates into “less.” The same numerical considerations are applicable to human resources: Armenia has 4.4 physicians per 1,000 people, while Canada, for example, has 2.6 for the same proportion, and Europe has 3.7. If assessments were hinged on considerations of such numerical superiority, then the quality of healthcare in Armenia would be better or commensurate to that of Europe or Canada. But this clearly is not the case: Armenia has more doctors per capita, yet has a much lower and diminished quality of care.
So what happens when you have such an overabundance of “hardware” in a resource-limited setting? As research demonstrates, it leads to some pretty disappointing results. The over-accumulation of hardware requires the maintenance and utilization of such hardware, which, needless to say, costs money. Combined with a grossly underfinanced healthcare system, Armenia now tops the list of countries with highest out-of-pocket health care spending in the world, with 84% of health expenditure coming straight from the patient or their families. And with most of this spending going towards high-level tertiary care, state institutions are left with practically nothing to build, maintain and improve a primary care system to keep its population healthy, to diagnose and prevent serious diseases early, and to manage chronic conditions well. With this perfect storm, the survival rates for conditions that could be prevented or treated early remain extremely low, while the risk of dying prematurely from manageable conditions remain quite high.
The Public
Any treatment of reforms at the institutional level must also be cognizant of the role that the public will play in the process, and in this context, it is important to note that no government can create adequate healthcare in the absence of the people’s willingness to contribute to their own well-being. The responsibility of each individual to contribute to their own health and to the health of the rest of society is of tremendous importance and can never be fully assumed by the government. However, the government can contribute to this process by enhancing health education, public information campaigns, and developing a culture of health promotion.
Since the objective is to have a society in good health, as well as a good healthcare system, it is critical to acknowledge the role of individuals and society in achieving this. Over-emphasizing the role of government in assuring a “good” healthcare system will not, in of itself, lead to good overall health outcomes. A simple analogy speaks to this: having the best fire response service in the world will not assure good outcomes if one keeps building houses that are unable to withstand the wind.
In the broader scheme of things, the general goal is two-fold: a) to produce and sustain a healthy population that is defined by maximization of quality of life and prolonged life-expectancy; and b) a healthcare system that minimizes the severity of illness or disability. An important mechanism of doing this is to enhance the health culture in Armenia that focuses not only on improving healthcare, but also improving health. Health here is specifically defined as a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Increasing public health requires improvements in three important sectors: public health infrastructure, primary health services, and increasing the role of individuals and civil society in health promotion.
These improvements in health, as discussed above, must be aligned with reforms within the healthcare system where the system is transformed into a sustainable and thriving sector. These reforms must include, but are not limited to, the following: adequate “surge capacity” to allow for Armenia to deal with natural and man-made disasters it is prone to; transformation of the country from a health solution consuming nation to a health solution producing nation; and development of robust research, education and innovation infrastructures.
Conclusion
As the quantitative metrics show, Armenia’s problem is no longer one of inadequate resources. Armenia’s health sector, generally speaking, has most of what it needs, and the Diaspora, when it comes to resource-accumulation, is the proverbial icing on the cake. Thus, what Armenia needs to focus on is the system, and the processes of good governance, leadership, prioritization, coordination, and collaboration that would allow it to put its resources to better and more effective use. If we want better medical education, we should improve the medical education system, not just give a lot of lectures. If we want better outcomes for our patients with cancer, we should seek to have a system that knows how to do that, not just do a lot more of the cancer surgeries. Simply put, the following question needs to be asked: What can we do to make the system work better, rather than engaging in yet another initiative that seeks to put a bandaid on a festering wound. To borrow from the adage, Armenia needs to treat the disease, not the symptoms.
—————————————-
[1] Examples include the Millennium and Sustainable Development Goals.
[2] Tamara Tonoyan and Lusine Muradyan. (2012). “Health Inequalities in Armenia-Analysis of Survey Results.” International Journal for Equity in Health. 11, Article 32.
[3] Dr. Shant Shekherdimian: Redefining Armenia-Diaspora Collaboration in Healthcare – YouTube.

Illustration by Harut Tumaghyan.
Public Health | Magazine Issue N13
Armenia’s healthcare system, for the last three decades, has suffered from an absence of vision, lack of strategic planning, poor quality and widespread corruption and nepotism. The country’s healthcare system, broadly speaking, is inefficient, relatively ineffective, and for these reasons has produced a less healthy population. In the wake of the COVID-19 pandemic and the 2020 Artsakh War, now more than ever, systemic reform in the healthcare sector must be a priority.

